AHP At-A-Glance
AHP Inside The Body
AHP Perspectives
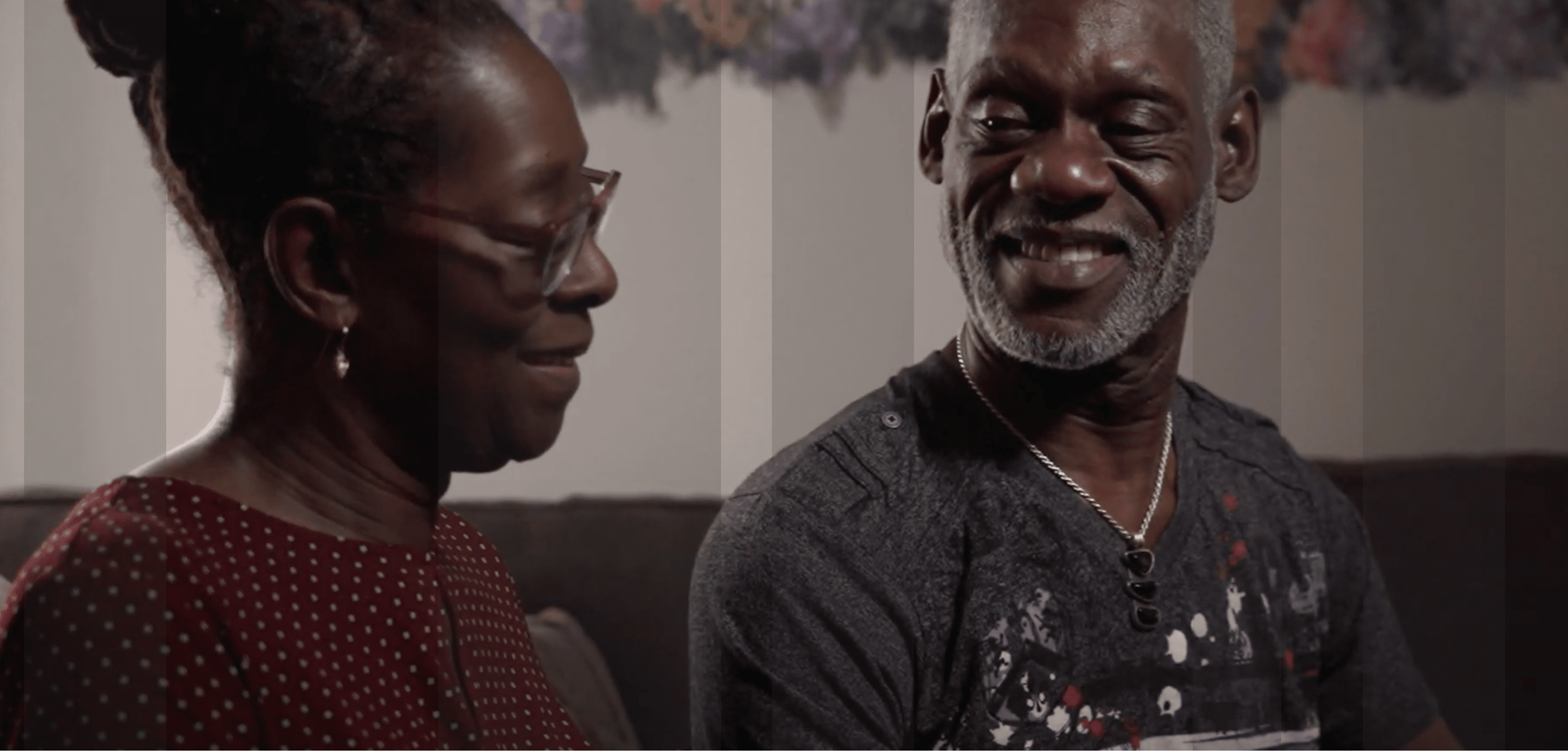
The pain caused by hereditary coproporphyria (HCP) is just something I wouldn’t want anyone to have to go through.
– Nathan, diagnosed with Hereditary Coproporphyria (HCP)
Additional Information
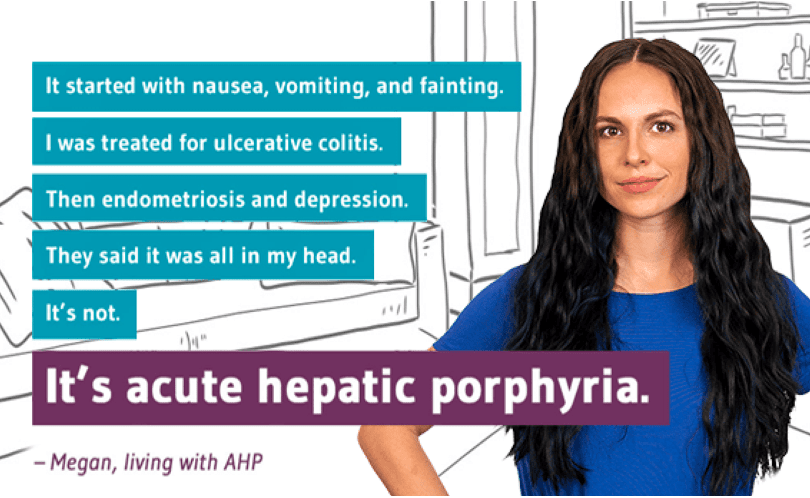
Pinpoint AHP®
Pinpoint AHP® provides patients and their caregivers a variety of resources to help them understand the types of acute hepatic porphyria (AHP) and recognize the signs and symptoms.
Alnylam Act®
Alnylam Act® provides no-charge independent genetic testing and counseling to individuals in the U.S. and Canada who may have porphyria.
Pinpoint AHP, Alnylam Act, and their associated logos are trademarks of Alnylam Pharmaceuticals, Inc. © 2023 Alnylam Pharmaceuticals, Inc. All rights reserved.

You will be redirected to an external site that may include social media, event registration, or other third-party content related to Alnylam.
Please note that these external sites have their own terms of service and privacy policies, which may differ from those of Alnylam.
Proceed to Site